
For women, deciding to have sex involves much more than the physical act itself. Their decision also includes the use of contraception and the best way to protect themselves and their partner against unwanted pregnancies. Finding what forms of contraception work for their bodies can be a complex, confusing, and exhausting process of trial-and-error. In many relationships, women carry the burden of prescription contraception, especially if partners refuse to use barrier methods such as condoms.1 Like cleaning or child rearing, contraceptive use is a taken for granted “form of domestic labor in which women routinely engage”. 2
The physical and emotional toll of birth control
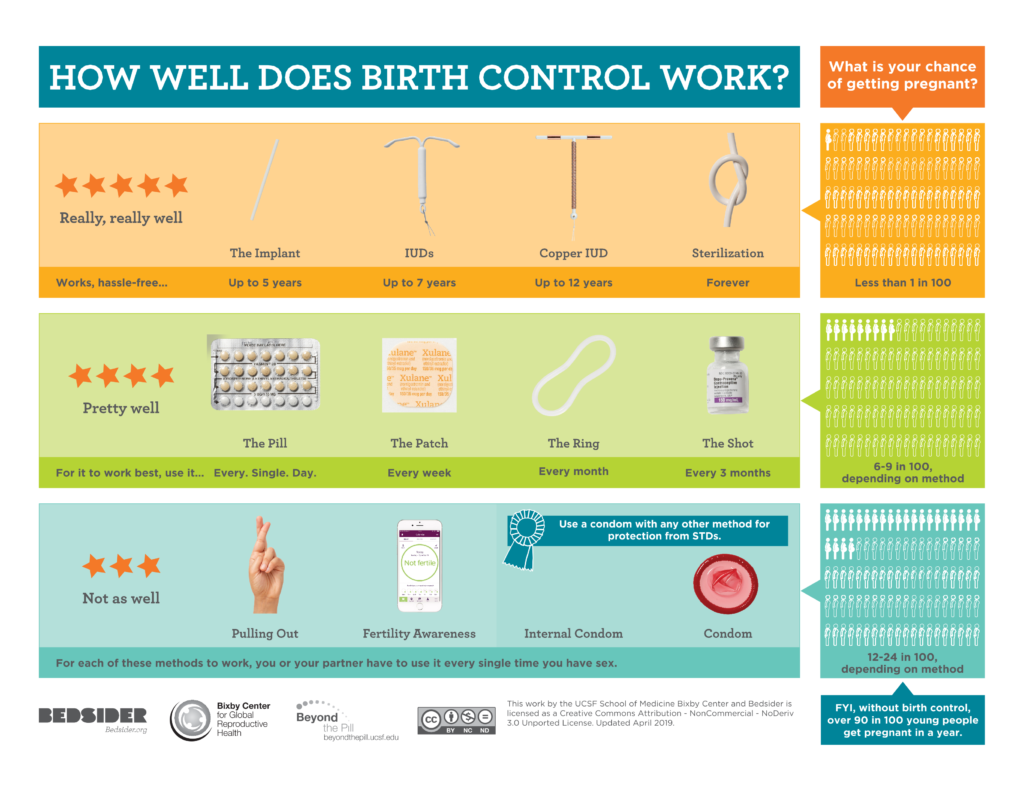
The societal expectation placed on cisgender women in heteronormative relationships to bear the burden of contraception results in many women spending their lives under the influence of synthetic hormones that threaten their mental and physical health. Many of the most effective contraceptives such as the pill, the patch, the ring, the implant, and the IUD use artificial hormones such as estrogen and progestin to prevent pregnancy. 3 Many methods come with a laundry list of side effects such as persistent headaches, nausea, weight gain, acne, depression, anxiety, and unpredictable bleeding. For many women, these side effects are life altering and significantly decrease their quality of life. Contraception also comes with significant health risks such as life threatening blood clots, an increased risk of breast cancer, ectopic pregnancy, and loss of fertility. 4.Over 85% of women in America have used some moderately effective form of birth control and nearly half of these users have discontinued their birth control because of dissatisfaction with side effects.5
The price of protection
Many women think the contraceptive counseling they receive from their doctors does not prepare them for the severity of the side effects they face.6 Reflecting on negative birth control experiences, many patients thought that doctors downplayed potential side effects when prescribing their birth control.7Even if side effects begin negatively impacting their daily life, doctors advise women to stick with their birth control method for at least 6 months before deciding it is not right for them. This illustrates how society normalizes side effects and sells them as the price of protection against pregnancy.8
When women attempt to challenge their doctors and nurse practitioners, their observations and concerns about their birth control are invalidated and deemed “informal knowledge”.9 Because of the tendency of medical professionals to disregard female experiences with contraception, women must perform additional labor of self advocacy to receive the care they require. 10
Devaluing experiences based on race and class
Women in historically marginalized groups are regularly characterized by medical professionals as less educated and uncredible reporters of their own concerns. Their rejection of birth control methods tend to be more scrutinized due to class discrimination and racism 11. Some physicians discredit women because of cultural stereotypes, blaming women’s complaints of side effects or concerns about birth control on “cultural superstitions and beliefs” 12. Racist stereotypes are prevalent in contraception consultation as medical workers characterize black women as financially irresponsible and likely to have children while poor 13. When it comes to birth control, discrimination places racially minoritized women in a particularly vulnerable position that puts their physical and mental health at risk.
Birth control as a shared responsibility
Although men and women both contribute to pregnancy, the responsibility for preventing unwanted pregnancies often falls on women. Birth control options for men remain severely limited. Development of a safe and effective birth control pill, implant, or injection for men has yet to be widely approved or distributed 14. There is a large amount of debate over hormonal birth control for men. This is largely due to concerns about side effects; many men worry that vasectomies or any form of hormonal birth control will decrease their libido, a side effect many forms of birth control have caused in women for years 15. Additionally, contraceptives for men are met with more resistance because they threaten sexual performance; something society ties closely to masculinity. At the end of the day, women’s mental and physical health becomes a casualty of societal resistance to male birth control. Will women always be expected to bear this burden alone? Maybe not. Growing knowledge of the male reproductive system, a political climate more accepting of male contraception, and increased funding for research are all a step towards the future development of male contraception 16. If progress continues, future generations of women may not need to shoulder the burden of birth control alone.
References
[1] Christensen, Damaris. 2000. “Male Choice: The Search for New Contraceptives for Men.” Science News, pp. 222.
[2] Elson, Jean. 2005. “The Male Pill: A Biography of a Technology in the Making.” Contemporary Sociology 34(2):201-203. doi: http://dx.doi.org/10.1177/009430610503400260.
[3] Kimport, Katrina. 2018. “More than a Physical Burden: Women’s Mental and Emotional Work in Preventing Pregnancy.” Null 55(9):1096-1105. doi: 10.1080/00224499.2017.1311834.
[4] Littlejohn, Krystale E. 2013. “”IT’S THOSE PILLS THAT ARE RUINING ME”: Gender and the Social Meanings of Hormonal Contraceptive Side Effects.” Gender & Society 27(6):843-863. doi: 10.1177/0891243213504033.
[5] Mann, Emily S. 2022. “The Power of Persuasion: Normative Accountability and Clinicians’ Practices of Contraceptive Counseling.” SSM – Qualitative Research in Health 2:100049. doi: https://doi.org/10.1016/j.ssmqr.2022.100049.
[6] Planned Parenthood. 2022. “Birth Control.”, Retrieved 4/1/, 2022.
[7] Stevens, Lindsay M. 2018. ““We have to be Mythbusters”: Clinician Attitudes about the Legitimacy of Patient Concerns and Dissatisfaction with Contraception.” Social Science & Medicine 212:145-152. doi: https://doi.org/10.1016/j.socscimed.2018.07.020.
[8] University of San Francisco School of Medicine Bixby Center, and Bedsider. 2019. “How Well Does Birth Control Work?”, Retrieved 4/10/, 2022.